This fact sheet gives you information about pre-implantation genetic testing of embryos if you are considering this as part of your IVF treatment. It explains what it is and who may benefit from this technology; what we can test for; and what IVF treatment using this approach involves.
What is genetic testing?
Pre-implantation genetic testing is a laboratory procedure that can be carried out as an add on to an IVF cycle. In addition to observing what the embryos look like and how they are developing, a genetic assessment of the embryos is performed that tells us which, if any, are carrying certain genetic errors so we can avoid transferring any of those embryos to the uterus.
There are a range of advanced testing methods available thanks to recent science and our partnership with leading genetic laboratories.
Testing is usually done at the blastocyst stage of the embryo’s development (around 5 days after fertilisation). (See separate Blastocyst culture fact sheet).
As you will need to wait for results of the tests, your embryos will be frozen until results are assessed and you decide to go ahead with a ‘Frozen Embryo Transfer’ cycle of IVF. (See separate FET fact sheet).
A little about chromosomes and genes
Understanding a little about chromosomes and genes will help you understand genetic testing.
In the nucleus of all our cells, our DNA is organised in string-like structures called chromosomes and these are made up of all of the instructions (genes) for creating a unique individual.
A human normally has 46 chromosomes in every cell (23 pairs) with one set coming from the mother’s egg and the other from the father’s sperm. The X and Y chromosomes are one of these pairs and determine the sex of the embryo.
When an egg and sperm come together at fertilisation, the combined set of chromosomes is inherited by every cell of the embryo and subsequently by all the cells of the body.
What can go wrong?
Problems with numbers
If there are errors in the number or structure of the chromosomes in the cells of an embryo, the chances of it progressing to a normal pregnancy and live birth are significantly reduced.
Where there are missing or extra chromosomes in an embryo (or an egg or sperm) we call these numerical errors aneuploidy. Aneuploidy can crop up unexpectedly in embryos, but it more commonly comes from the egg or sperm from which the embryo was derived. If there are extra or missing chromosomes in an egg or sperm the resulting embryo will also be aneuploid.
It is known that aneuploidy accounts for why many embryos don’t result in pregnancy, or if they do, the pregnancy miscarries. In addition, the rare aneuploid pregnancies that do reach birth will be affected by conditions such as Down Syndrome.
Aneuploidy is particularly relevant for women as they get older because we know that the frequency of aneuploidy in eggs increases with age and this is a major contributing factor to the age-related decline in women’s fertility.
Problems with structure
Some people also carry structural errors in their chromosomes where pieces of two different chromosomes have become swapped round or one part of one chromosome has been turned upside down. These ‘translocations’ and ‘inversions’ may not affect the person themselves, but they do often affect their embryos because their eggs or sperm (and resulting embryos) may not have a complete set of chromosomes. Again such embryos will not implant, will miscarry or can (rarely) result in the birth of an affected individual.
Problem genes
We have two copies of every gene in our cells and some people are affected by serious errors (mutations) in certain genes. Others may know that, even though they themselves are not affected, one of their copies of a gene is faulty and they are ‘carriers’ for this mutation.
In either case, they may be very likely to pass that mutation on through their eggs or sperm and have children that are affected by a serious genetic condition. Over 4000 human diseases are known to be caused by these ‘single gene disorders’ and they include sickle cell anaemia, haemophilia, cystic fibrosis and Huntington’s Disease.
Who can benefit from genetic testing?
There is a range of reasons why your doctor might recommend genetically testing your embryos. Situations where the doctor may recommend that we check the number of chromosomes in the embryo include:
- An ongoing problem with embryos failing to implant or repeated miscarriages, where we suspect errors in the number of chromosomes may be contributing.
- A previous pregnancy or birth affected by a chromosomal abnormality.
- A woman whose age is likely to be causing an increase in errors in the number of chromosomes in embryos and also increasing the chances of having a child affected by conditions such as Down’s Syndrome.
- Where it is necessary to determine the sex of an embryo because there is a risk of passing on a specific disorder to children of one sex. It’s important to be aware that unless there is a serious medical reason for doing this, IVF clinics in Australia cannot otherwise disclose the sex of an embryo.
In addition to checking the number of chromosomes, the doctor may recommend testing embryos for specific problems where it is known that:
- A chromosome structural rearrangement (translocation or inversion) that is carried by one of the parents is preventing pregnancy, causing miscarriage and /or risks affecting children.
- There is a risk of passing on a specific single gene disorder or condition to children.
When do we decide about genetic testing?
You should ideally start considering genetic testing and speak to your Life Fertility Clinic specialist well before you want to have your IVF treatment as it can take a number of months to assess your needs, confirm that testing is possible for you, arrange the screening and take preliminary blood and DNA tests from both parents.
If you are going to have genetic testing, you also need to talk to one of our scientists and to see a Genetic Counsellor to discuss all the issues.
What types of genetic tests are available at Life Fertility Clinic?
Chromosome testing
When we want to assess the number of chromosomes in the embryo, this is commonly referred to as Pre-implantation Genetic Screening (PGS).
There are various methods available for assessing the number or structure of chromosomes in embryos. The lab technique that is used by the genetics laboratory used by Life Fertility Clinic is called Next Generation Sequencing (NGS).
In most cases NGS is also the technology used if we also want to test your embryos for a specific structural chromosome problem (translocation / inversion). In these cases, before you start your treatment cycle, the genetics lab will evaluate your condition and make sure that they will be able to reliably identify affected embryos for you. Sometimes this evaluation can delay or prevent treatment and / or alternative testing methods might need to be used. Your Life Fertility Clinic scientist will explain this ‘feasibility assessment’ process to you.
Single Gene testing
When we want to test embryos for a disease caused by a single mutant gene, this is commonly referred to a Pre-implantation Genetic Diagnosis (PGD).
The lab technique used by the genetics lab to detect these disorders is called karyo-mapping.
Before you start your treatment cycle, the genetics lab will first work out whether karyo-mapping is going to be able to reliably detect your specific abnormal gene in your embryos. This ‘karyo-mapping evaluation’ process can take a few months and you and various family members will need to provide blood samples. Your Life Fertility Clinic scientist will explain this ‘karyo-mapping evaluation’ process to you.
What does a PGS or PGD cycle actually involve?
Once all the preliminary evaluation and genetic counselling has been completed, a PGS or PGD cycle is very like a regular IVF cycle (see separate IVF fact sheet) for the couple themselves.
We inseminate the eggs using ICSI (see separate fact sheet) and fertilised eggs are cultured to the blastocyst stage, up to day 6 after fertilisation.
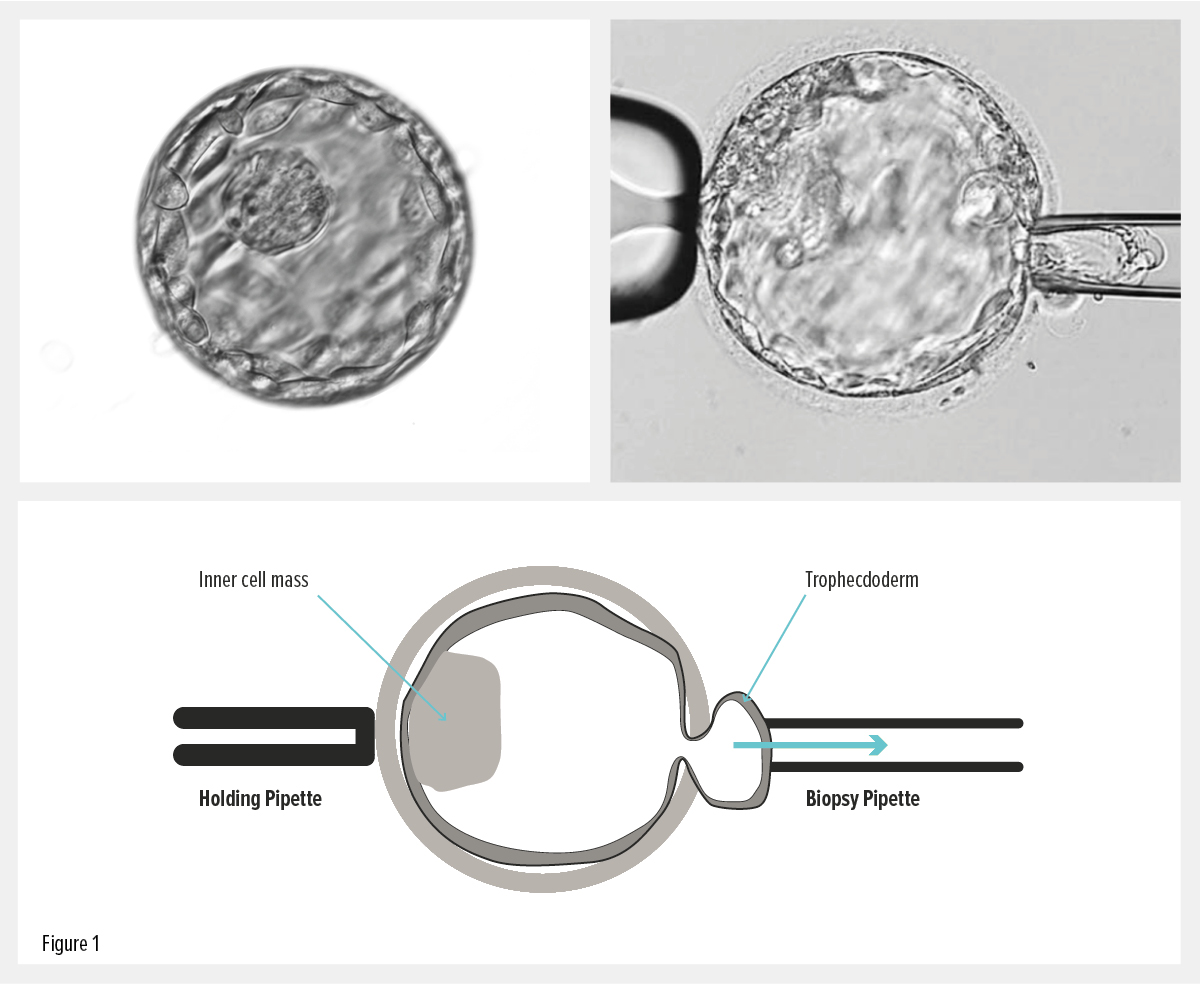
At this stage the scientist very carefully takes (biopsies) a few cells from each suitable embryo (see fig 1) and those cells are sent to the genetics team for testing.
Figure 1: The blastocyst stage embryo is picked up using very small tools (pipettes) and a few cells from the outer layer (the trophectoderm) are removed as they emerge through a hole in the surrounding shell.
The genetic testing process takes a few weeks so the embryos are frozen immediately after biopsy.
When we have the results and have identified an embryo suitable for transfer, your cycle will be completed later with a ‘Frozen Embryo Transfer’ cycle (see separate fact sheet).
Does the biopsy harm the embryos?
We take the utmost care with biopsies and we only test embryos that are good quality and appear suitable for biopsy.
One of the reasons that we recommend biopsy at the blastocyst stage is that the medical literature suggests that a biopsy at this stage is less damaging to the continuing development of the embryo than biopsy at other stages. There is however still a chance that an embryo may fail to survive the process. We estimate that the chance of this happening is less than 1 in 20.
Are there any other hurdles?
- One of the hurdles for many couples is getting to the point of having embryos to biopsy in the first place. Patients who have previously had low numbers of eggs or good quality blastocysts may only have a few (or no) embryos to biopsy. Your Life Fertility Clinic doctor or scientist will discuss these issues with you.
- Even if we manage to take a good biopsy from an embryo, there is a chance that technical difficulties may prevent the laboratory completing tests successfully and the result will come back as ‘failed’. In addition, results for some embryos may be inconclusive for some parts of the test. You should consider how you will feel about failed or inconclusive results and what action you might want to take with the embryos.
- Another possible hurdle is the freezing and thawing process. Although the biopsy process doesn’t seem to affect the embryo’s ability to survive, there will always be some blastocysts that don’t survive. We estimate that this occurs in about 1 in 20 blastocysts.
How reliable are the test results?
Although pre-implantation testing results are generally good, they are not 100% accurate and are not an absolute guarantee that an embryo with an abnormality won’t be transferred or form a pregnancy. Although the incidence in blastocysts is low, some embryos may be ‘mosaic’, which means there are cells with different genetics within the same embryo and the biopsied cells might not be a true representative of other cells in the embryo.
It is also important to remember that we are only assessing the number of chromosomes in the cells of the embryos and/or the particular structural abnormality or single-gene that is relevant to you. We are not testing for any other abnormalities.
We recommend that, if genetic diseases or chromosomal conditions are a critical factor for you, you should also have prenatal testing if you become pregnant in order to confirm the early genetic testing.
What next?
Because genetic testing is not a perfect science and because it may lead to difficult decisions for potential parents, it is important to consider it carefully before you start IVF.
Your Life Fertility Clinic doctor will help you consider the pros and cons for your particular situation. At Life Fertility Clinic we have also made it compulsory to have an education session with one of our scientists and a session with a Genetic Counsellor before you decide to have pre-implantation genetic testing so you have a chance to consider all the possible options and outcomes.
Once you are ready to go ahead, your Life Fertility Clinic Nurse Coordinator will arrange the preliminary tests, necessary consent forms and explain the next steps.
Contact Life Fertility Clinic
The friendly and professional team at Life Fertility Clinic are happy to answer any other questions you may have about genetic testing.
